Common Questions About Lynch Syndrome
Explore answers to the most frequently asked questions about Lynch syndrome, a hereditary condition that increases cancer risk. Always consult your doctor for medical advice.
What is Lynch Syndrome?
Lynch Syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC), is a genetic disorder that increases the risk of colorectal cancer and other types of cancer. It is caused by inherited mutations in mismatch repair genes.
I suspect I may have Lynch Syndrome, what should I do?
If you suspect that you may have Lynch syndrome, it’s important to take the next steps toward understanding your health and managing any potential risks. Here’s a guide on what to do:
1. Speak with Your Doctor
- Consult a healthcare professional: The first step is to talk to your primary care doctor or a genetic counselor. If you have a family history of cancers associated with Lynch syndrome (e.g., colorectal, endometrial, ovarian, or other cancers), this can help guide the discussion.
- Explain your concerns: Share your family history of cancer or any other symptoms you’re experiencing, as this could indicate a higher likelihood of Lynch syndrome. Your doctor may refer you to a genetic counselor for further evaluation.
2. Genetic Testing
- Genetic Counseling: If your doctor suspects you might have Lynch syndrome, they will likely refer you to a genetic counselor. Genetic counselors help assess your family history and explain the potential benefits and risks of genetic testing.
- Genetic Testing: Genetic tests are available to determine if you have mutations in specific genes associated with Lynch syndrome (such as MLH1, MSH2, MSH6, PMS2, or EPCAM). The test usually involves a blood or saliva sample.
3. Understanding the Results
- Positive Test: If you test positive for a Lynch syndrome-related mutation, your doctor will help guide you through a management plan, which may include more frequent cancer screenings and discussions about preventive options. Also consider cascade testing for your family.
- Negative Test: If the test is negative, it means you do not have the gene mutation associated with Lynch syndrome, but if you still have a family history of cancer, further steps may be necessary to monitor your health.
How is Lynch Syndrome diagnosed?
Lynch Syndrome is diagnosed with a blood test or salvia sample with genetic testing. This test looks for mutations in specific genes associated with the condition. Family history and clinical criteria are also considered.
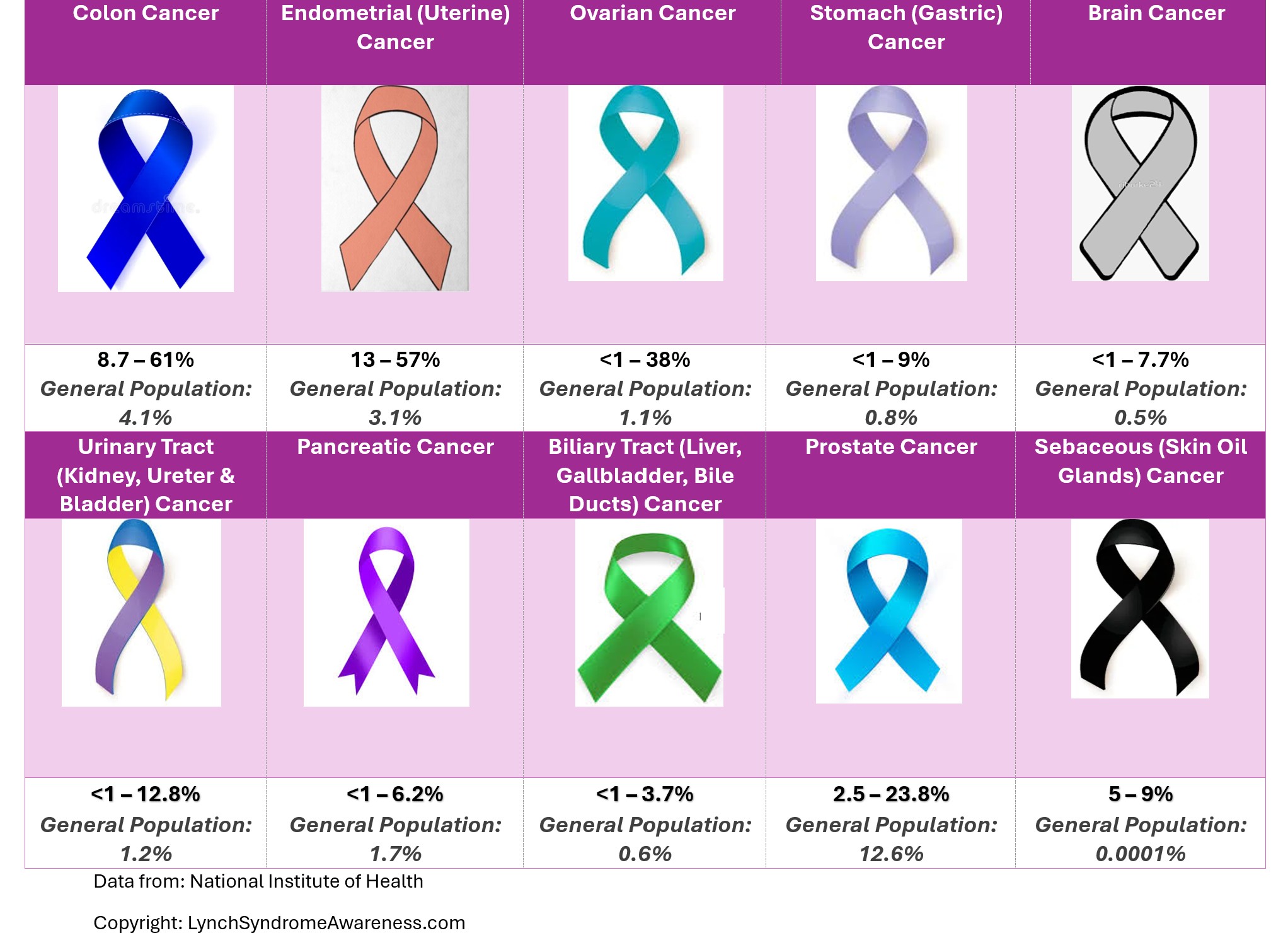
What are the cancers associated with Lynch Syndrome?
Individuals with Lynch syndrome and which mutation have a higher risk of developing cancer. These may include colorectal cancer, endometrial cancer, ovarian, gastric, urinary tract, biliary tract, prostate, pancreatic, brain, and skin cancers.
What are the types of mutations associated with Lynch Syndrome?
The five types of mutations associated with Lynch Syndrome are MLH1,MSH2,MSH6,PMS2, and EPCAM:
If I am diagnosed with Lynch Syndrome, are my children and family at risk?
Yes, your children and some family members have a 50% chance of inheriting Lynch Syndrome. These family members include parents, siblings, aunts, uncles, nieces, nephews, and cousins. Please encourage all of these family members to seek Genetic Counseling.
What screenings are recommended for patients with Lynch Syndrome?
Each of the mutations have different guidelines, but these are some of the most common.
-High definition Colonoscopy every 1-2 years starting in the 20’s.
-Endometrial biopsy every 2-3 years
-Annual blood tests
-Urine tests
-Annual skin screenings
Does having Lynch Syndrome mean that I will definitely get cancer?
No, having Lynch Syndrome doesn’t mean you will get cancer. However, it does increase your risk. Lynch Syndrome is a genetic condition that increases the risk of developing certain cancers.
Is there a CURE for Lynch Syndrome?
Currently, there is no cure for Lynch syndrome, but it is a condition that can be managed with regular monitoring and preventive measures.
While it can’t be “cured” in the traditional sense, there are several ways to manage the risk associated with Lynch syndrome:
-
Preventive surgery: In some cases, individuals with Lynch syndrome may opt for preventive surgeries, such as the removal of the colon (colectomy) or the removal of the uterus and ovaries (hysterectomy and oophorectomy) to reduce the risk of certain cancers.
-
Medications: There are ongoing studies into the use of medications that might reduce cancer risk for people with Lynch syndrome. Some medications, like aspirin, have shown potential in reducing colorectal cancer risk, but more research is needed.
-
Genetic counseling: Genetic counseling and testing are important to understand the risks and make informed decisions about surveillance and preventive options for both affected individuals and their family members.
If you or someone you know has Lynch syndrome, it’s essential to work closely with healthcare providers to develop a personalized plan for managing the condition.
What are the latest advances for Lynch Syndrome?
Recent research has led to significant advancements in the understanding and management of Lynch syndrome, a genetic condition that heightens the risk of various cancers. Notable developments include:
-
Immunotherapy for Cancer Prevention: Studies have demonstrated that immunotherapy drugs, particularly checkpoint inhibitors, may prevent tumor development in individuals with Lynch syndrome. These treatments work by enhancing the immune system’s ability to identify and eliminate potential cancer cells before they form tumors.
-
Aspirin as a Preventive Measure: Clinical trials have indicated that regular aspirin use can reduce the risk of developing certain cancers in Lynch syndrome carriers. Aspirin’s potential benefits are thought to arise from its ability to activate specific immune responses that target and destroy precancerous cells.
-
Development of Preventive Vaccines: Researchers are exploring vaccines aimed at preventing cancers associated with Lynch syndrome. For instance, scientists from the University of Oxford, supported by Cancer Research UK, have initiated development of a vaccine named LynchVax. While clinical trials are not yet underway, this represents a promising step toward proactive cancer prevention strategies for those with Lynch syndrome.
These advancements offer hope for improved prevention and management strategies for individuals affected by Lynch syndrome.

With Lynch Syndrome, MMR genes refer to a group of Mismatch Repair genes that are involved in the correction of errors that occur during DNA replication. These errors, or mismatches, are typically small changes in the DNA sequence that occur when DNA is copied. Normally, those who are not affected by Lynch Syndrome mutations the mismatch repair systems will correct these errors, preventing mutations from accumulating.
In Lynch Syndrome (also known as Hereditary Non-Polyposis Colorectal Cancer or HNPCC), there is a genetic predisposition to cancer due to inherited mutations in certain MMR genes. These mutations lead to the loss of function in the mismatch repair system, which causes microsatellite instability (MSI) and an increased risk of cancer.
This website is intended for informational purposes only and is not a substitute for professional medical advice, diagnosis or treatment. Please talk to your healthcare provider about any questions or concerns you may have regarding your health.